Overview
Hyperparathyroidism (HPT) is characterised by an increased level of parathyroid hormone (PTH) in the blood. Increased levels of PTH cause serum calcium levels to increase and phosphate levels to fall. It can be divided according to its aetiology:
- Primary HPT:
- The disorder is from within the parathyroid glands themselves
- Secondary HPT:
- The disorder is from somewhere else outside the parathyroid glands
- This is usually in response to low calcium secondary to kidney, liver, or bowel disease
- Tertiary HPT:
- Usually seen in those with long-term secondary HPT. Eventually, this leads to parathyroid hyperplasia and autonomous PTH secretion
Calcium and phosphate homeostasis
PTH normally stimulates bone resorption, along with stimulating the kidneys to reabsorb calcium and convert 25-hydroxyvitamin D3 to its active form 1,25-hydroxyvitamin D3, which is responsible for the intestinal absorption of calcium. Low serum calcium stimulates PTH secretion, whereas high calcium levels suppress PTH secretion.
PTH reduces the reabsorption of phosphate from the proximal tubules in the kidneys, leading to more phosphate excretion in the urine.
Calcitonin is a hormone that opposes the effects of PTH and reduces serum calcium. It is released by thyroid parafollicular cells.
Chronic kidney disease and secondary HPT
Patients with chronic kidney disease (CKD) excrete less phosphate due to dysfunction of the kidneys. This leads to the removal of calcium ions from the circulation as they are deposited in the insoluble salt calcium phosphate. This leads to hypocalcaemia and an increased level of potassium ions in the circulation, leading to secondary hyperparathyroidism.
Epidemiology
- Primary HPT is the 3rd most common endocrine disorder
- Twice as common in women than in men
- Usually seen in people aged 50-60 years
Causes
Primary hyperparathyroidism
- Solitary parathyroid adenoma – 80% of cases
- Parathyroid hyperplasia
- Multiple parathyroid adenomas
- Parathyroid malignancy
Secondary hyperparathyroidism
- Chronic kidney disease
- Calcium loss/increased calcium demand
Tertiary hyperparathyroidism
- Usually seen in those with long-term secondary HPT
- Eventually, this leads to parathyroid hyperplasia and autonomous PTH secretion.
Risk Factors
Primary hyperparathyroidism
- Aged 50-60 years
- Female sex
- Family history
- Multiple endocrine neoplasia (MEN 1 or 2A)
Secondary hyperparathyroidism
- Chronic kidney disease
- Any other cause of vitamin D deficiency (e.g. inadequate sunlight exposure/malabsorption)
Tertiary hyperparathyroidism
- Long-term history of secondary HPT
Presentation
Primary hyperparathyroidism
The features of primary HPT and hypercalcaemia can be remembered using the mnemonic:
- Bones – bone pain and fractures
- Stones – renal stones
- Abdominal groans – anorexia, nausea
- Psychiatric moans – depression, insomnia, impaired memory
- Thrones – constipation
- An ECG may show QT interval shortening
Secondary hyperparathyroidism
- Features of hypercalcaemia (mentioned above)
- Features of chronic kidney disease
- Features of malabsorption (e.g. coeliac disease, Crohn’s disease, chronic pancreatitis)
- Features of osteomalacia (e.g. bone pain, fractures, or bowed legs in children)
- Features of hypocalcaemia
Tertiary hyperparathyroidism
- Features of hypercalcaemia (mentioned above)
- Features of a condition causing secondary hyperparathyroidism
Investigations
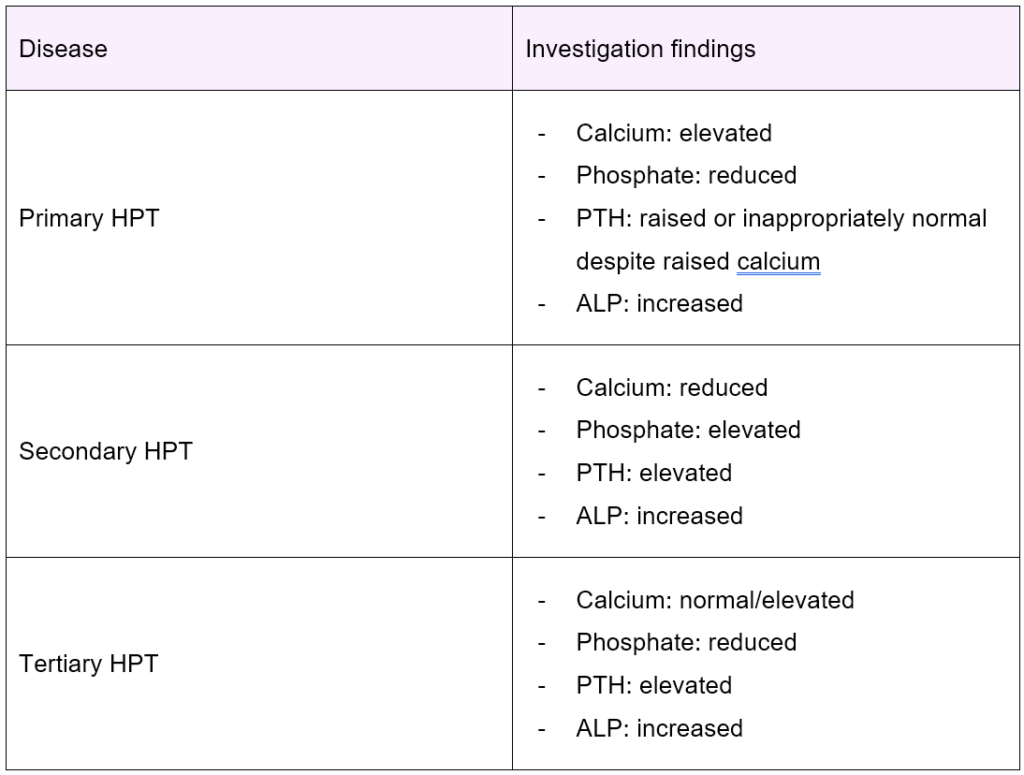
- Serum calcium:
- Findings vary depending on the type of HPT
- Serum phosphate:
- Findings vary depending on the type of HPT
- Parathyroid hormone:
- Findings vary depending on the type of HPT
- Alkaline phosphatase (ALP):
- Generally raised
- X-ray:
- May show pepper pot skull (salt and pepper sign) in the skull – these are multiple small well-defined areas of lucency in the skull cap
Management
Primary hyperparathyroidism
- 1st-line: total parathyroidectomy
- If unsuitable for/declines surgery: manage medically with calcimimetic (e.g. cinacalcet)
- Cinacalcet binds to calcium-sensing receptors leading to the reduction of serum calcium and PTH – it mimics the effects of calcium
Secondary hyperparathyroidism
- 1st-line: manage underlying cause (e.g. offer vitamin D and calcium supplements for a patient with CKD)
Tertiary hyperparathyroidism
- 1st-line: watch and wait + consider partial/total parathyroidectomy
Complications
- Osteoporosis
- Bone fractures
- Renal stones
- Features of hypercalcaemia (e.g. depression, constipation, nausea)
- Complications of surgery:
- Hypocalcaemia
- Recurrent laryngeal nerve palsy
- Haematoma formation and airway obstruction